Attachment Considerations, Options and Selection Part I
By: Chris Bormes
Editor’s Note: This blog is a special two-part feature.
The opportunity to write this blog for NADL is an honor. This is a huge topic, and I struggle to get all of these points across in an eight-hour course, so I will do my best to do so in 1500 words.
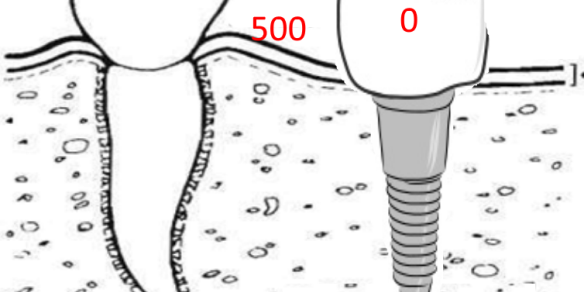
Initially, with the edentulous patient who will receive an implant supported or retained prosthesis, we need to recognize the difference between natural teeth and implants. Natural teeth have periodontal ligament, nature’s shock absorbers. When patients come into occlusion, there may be up to 1mm of movement between opposing natural teeth. Implants do not have these shock absorbers, and we therefore need to protect our implants. I like to use the analogy of driving a truck down a road with potholes—the natural tooth side has shocks, and the implant side does not.
Further, natural teeth provide proprioception, which protects the teeth by providing neurological stimulus letting the brain know if we are overloading or potentially damaging the tooth prior to completion of the destructive movement. Teeth are sensory organs, and the tactile sensory feedback coordinates chewing, swallowing, and breathing. The only tactile sensation available to implant restorations comes from bone deformation, which results in a threshold level 50 times greater than that of the natural dentition2.
The absence of mechanoreceptors impairs fine motor control by a reduced feedback mechanism. Studies also show that subjects with dentures and implants are unable to position their jaws as precisely as those with natural teeth. This lack of positional control, coupled with increased tactile sensory thresholds, results in much greater force being applied to implant restorations versus tooth-borne prosthetics.3
Therefore, implant prosthetics are likely to experience a greater incidence of mechanical damage… implant-supported fixed hybrid prostheses experience 3.8 times more prosthetic complications than biologic complications.4 Therefore, it is important to design a prosthesis that may be serviced and repaired as the patient ages and needs change.


When choosing the appropriate restoration, opposing arch force, interocclusal space, bone quality, patient health and dexterity (hygiene), pictures and vides of function, speech and smile line (gingival transition), parafunctional movements, and most importantly, patient expectations and desires all need to be reviewed by the restorative team.
Since today’s message is choosing the correct attachment, we are going to make the assumption that we are not providing a full arch Fixed Detachable (hybrid) restoration because a) the patient had a high, medium, or gummy smile line and removing bone to place the implants above the prosthesis tissue junction was not an option; b) the patient needed a flange to restore lip contours and a youthful appearance; and/or c) the patient did not have either the necessary dexterity now—or in the future—to clean the prosthesis.



The decision has been made to provide the patient with a removable prosthesis, and we can go back to our checklist of criteria to assist us in deciding between a bar and stud overdenture.
A CBCT scan is key to identifying how many—and where—we can place our implants to decide if this will be 100% implant supported (rigid, non-moving), or a combination of implant and tissue supported (resilient, moving) prosthesis.
Another key will be understanding the difference in bone quality in the mandible and maxillae. In general, bone is 50% more dense in the mandible than in the maxillae, providing support for greater opposing forces. It is one of the driving factors to place bars in the maxillae as opposed to studs—the bar connects our weaker implants together, better distributing opposing forces.
Goodacre and Kan have shown that overdenture restorations in the maxillae have a 78.7% implant survival rate (0-10 years) compared to 95% in mandibular bone.


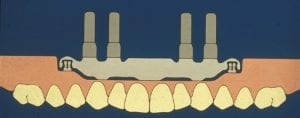
Our goal is to restore as much function as possible for our edentulous patients, and if we have enough well placed implants to fully support the prosthesis, a Bar overdenture is the best option. This is a rigid, no moving restoration—feels fixed to the patient—yet can be removed for easy cleaning, can have a flange for esthetics, and can be independently serviced.
Independently serviced is a major advantage of a rigid overdenture bar compared to a fixed detachable. If there is an issue that requires servicing with a fixed detachable, the entire restoration must be removed—composite removed, teflon tape pulled out, and each screw removed to service the prosthesis.
Conversely, if a Hader Bar overdenture feels loose, an assistant may simply remove the prosthesis and replace the Hader clip in seconds—easy servicing and time saving for both patient and clinician. Further, a patient is more likely to come in for a 30 minute servicing appointment than a 2 hour removal and cleaning of a fixed prosthesis.

Bars provide splinting (protection in the maxillae), can accommodate divergent implants, and provide great prosthesis stability.

If the case is going to be a combination of abutment and tissue supported prosthesis, a bar or stud can be used. Think of a two implant mandibular overdenture. A huge factor in your decision to choose bar or stud needs to be the the residual ridge.


The flanges of the denture will be able to provide great stability for a patient with a taller ridge. You can place a super resilient attachment—think an O-ring—here and the patient will have both support, stability, and retention. However, if the ridge has atrophed, and is “pancaked”, there will be zero prosthesis stability. If we placed O-rings on this patient, due to the lack of posterior stability, the patient would be coming in to our practice all the time complaining that the “attachments feel loose”. Even if you used super strong 8lb Locator attachments, it would still “feel loose” because of the lack of prosthesis stability.
Remember, stability of the denture has a stronger influence on patient satisfaction than retention.
If we have chosen a bar that will be a combination of abutment (anterior) and tissue supported (posterior), we need to choose a design or retainer that will provide either a vertical, rotational, or hinge movement to protect our abutments as the prosthesis goes from abutment to tissue supported during function (chewing, swallowing, etc).

Chris Bormes graduated from Gonzaga University prior to attending the Dental Laboratory Technology program at City College of San Francisco. Chris has earned both ICOI Fellowship and Mastership in Dental Technology; graduated from both Ticonium’s and Bego’s Partial Denture Programs; is a candidate for CDT in Complete Dentures; wrote the PREAT Corporation Technical Manual, and has invented 6 different attachments. Chris has lectured both nationally and internationally and is recognized as an expert in attachments and implantology. Chris joined PREAT Corporation in 1997 and was named President in 2010. In 2017 alone, Chris Bormes held 25 courses for continuing education credit at both large conferences such as the annual Hinnman conference, DLOAC Dental Lab & CAD/CAM Annual Expo, and LMT Lab Days as well as local study groups. Chris Bormes is dedicated to non-commercial education with the sole focus of increasing the knowledge and skills of dentists in order for them to provide the highest quality of care to their patients.
Continuing education courses held by Chris Bormes are specific to treatment planning for patients involving removable prosthetics, overdentures, attachments, and implant supported and retained restorations. This includes educating dentists on ongoing treatment options, protocols, and technical developments in the dental industry based on sound scientific evidence. As patient-specific treatment options continue to evolve, the Chris Bormes will teach when, where, and how to informatively choose the appropriate treatment option specific to each patient.
As President & CEO, Chris leads a team of dental professionals committed to providing the highest quality parts, expertise, education, and service to our dental partners in order to improve the quality of life for all involved






Nice Article. Thanks for sharing. This is really helpful to people who don’t know about dental attachments. Keep posting.
Really a very helpful article thanks for sharing and keep on sharing
Oral Health Overall Health
Amazing Articles and blog posts on your website, Cards Dental also trying hard to deliver some information to dentists and patients on a daily basis.