Implant denture prosthesis utilizing hybrid technology has become increasingly more popular and successful for clinicians. But accurate and successful case planning on these types of cases includes detecting any existing patient problems before the treatment has started. We must anticipate the final outcome before the patient starts their treatment. This includes the important collaboration between the Oral Surgeon, Periodontist, General Dentist and Certified Dental Technician.
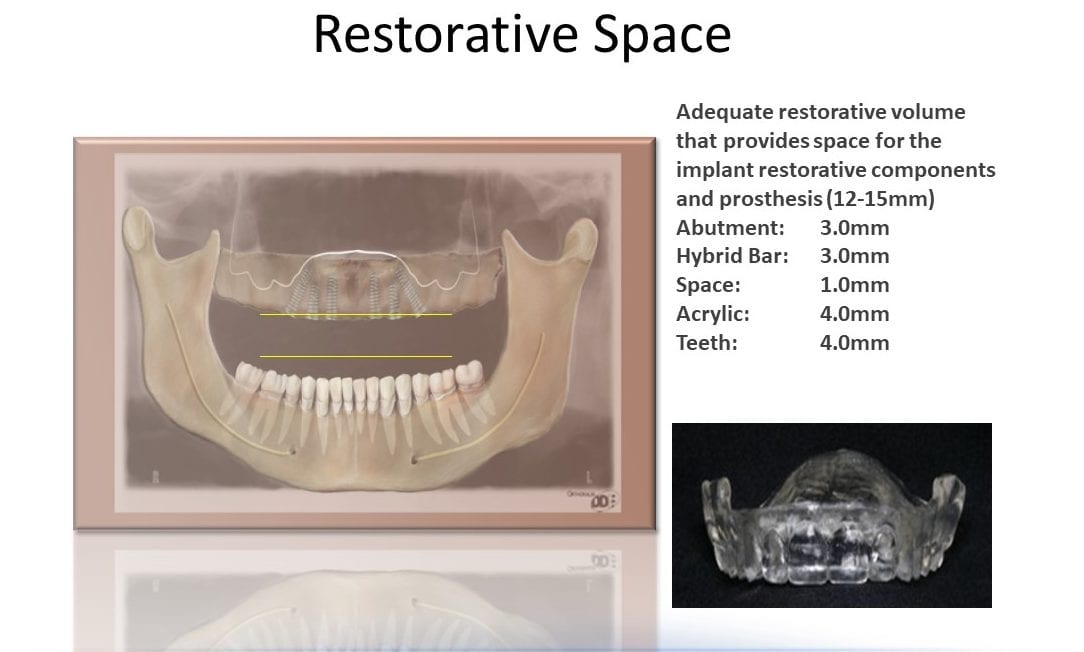
Case planning for these high-end esthetic cases requires a diagnosis of evident information received from the examination of the patient. We need to analyze restorative space measured from the implant to the opposing occlusion. Another necessary analysis in the amount of intra-occlusal space, keeping in mind implant components, hybrid bar, acrylic resin and denture teeth. (Photo 1). Adequate restorative volume that provides space for the implant restorative components is 12-15mm. Ideally, this is broken down for the following parts: Abutment 3.0mm, hybrid Bar 3.0mm, Space 1.0mm, Acrylic 4.0mm, Teeth 4.0mm. So, if we have intra-arch space of 30mm or more we will be planning a case which is reasonable to construct with a positive outcome. A realistic approach with reasonable patient expectations and treatment outcome must be addressed on the onset of the case so there are no negative surprises for the patient when the case in inserted.
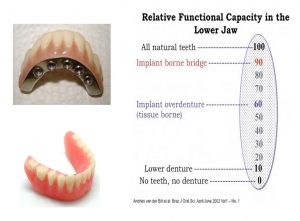
Let’s look at the relative functional capacity of the lower jaw (Photo 2). When we look at a lower denture the percentage goes down to 10% functionality. A hybrid type case raises this percentage to 90% functionality and an implant overdenture is at 60% functional capacity. Also needed for consideration is adequate coverage of the transition zone or high smile line for the patient. If a patient has severe recession and a Hybrid type case is not going to be esthetic enough to compensate for adequate build-up of the gingiva, then an implant overdenture must be considered.
Other considerations and treatment precautions for hybrid dentures are poor bone quantity, parafunctional habits and systemic health complications such as bleeding disorder, metabolic diseases or a compromised immune system.
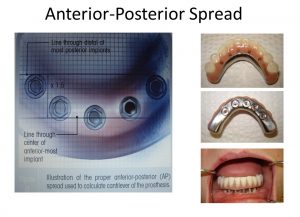
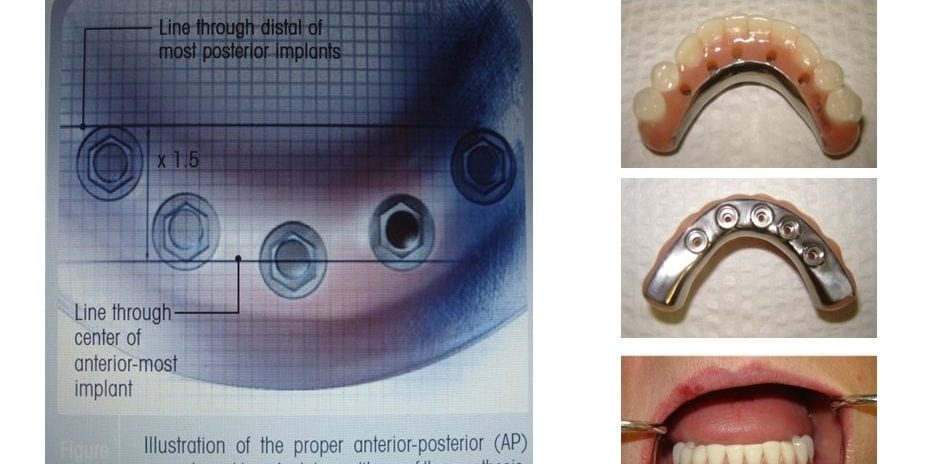
So why a hybrid denture? If a patient has a history of soreness, poor functionality and discomfort with an existing denture and the patient meets all the criteria for a hybrid denture, then this is a great option. If a patient’s natural dentition is in question and the patient desires stability, esthetics and function while meeting all the required criteria, then this patient is also a good candidate. In addition, a bar can achieve evenly distributed forces between the implants relieving any off-axis stress on the implant which can cause implant failure. Edentulous patients expect posterior first molar occlusion. Treatment planning the position of the implants and following the protocol of AP Anterior Posterior spread can achieve this result. Measure the distance in millimeters between the anterior implant and most posterior implants. Take the measurement and multiply by 1.5. This number offers you the distance that teeth can be cantilevered off the most distal implants (Photo 3).
Now let’s go to the beginning of the case and start the case planning. On the onset, implant planning and placement with a surgical guide and an appropriate software program is a must. We may be confronted with either an existing denture situation or an immediate denture case scenario. Either way we still must follow the correct protocol. Our object is to convert an existing denture or an immediate denture over to a temporary screw retained denture. We can even mill a provisional PMMA prosthesis instead of utilizing a denture if preferred. Once the screw retained temporary prosthesis is placed, on an average the patient will wait about six months to start the planning and fabrication of the hybrid denture.
Most of the cases that have seen a high success rate have been with at least 6 implants place on the maxilla ridge and 4 implants place on the mandibular ridge. If 4 implants are prescribed on the upper, then the posterior-most implants must be tilted at 45 degrees or less. Bone grafting is avoided by tilting the implants and utilizing available bone. Vertical placement of implants can be utilized with 6 or more implants.
At the point of preparing for the provisional denture, we must follow the traditional protocol, including preliminary impressions, final impressions utilizing a custom tray or the existing denture, proper occlusal records, denture set-up and try-in and the appropriate denture teeth and acrylic.
So, what is the dental laboratory’s role? The laboratory will work closely with the surgeon, general dentist and implant company on case planning. On the day of the denture conversion, the laboratory will provide chairside support in the conversion process converting a removable prosthesis over to a screw retained denture and then confirming future case planning regarding the milled hybrid bar prosthesis. If the clinician does not want chairside support, the laboratory will convert the denture in the lab utilizing a master model with proper implant placement information.
After all implants have osseointegrated and the surgeon and patient are satisfied to move forward with the hybrid denture, the planning can start with the proper protocol for the final screw retained hybrid denture (Photo 4). We’ll start with a preliminary impression and then make a custom tray having the doctor pick up the impression copings in the final impression. In many instances, the laboratory will make a clear duplicate of the denture for the day of the conversion and then the doctor can take a final impression at that time. When we receive the impression back at the lab, the technician will pour a soft tissue model and use this as the master cast. For the next patient visit, the technician will make a base plate and bite rim incorporating one or two temporary cylinders into the base plate ensuring stability when the bite registration is taken. At that same visit, a verification index will be utilized to verify that the impression and master cast are accurate.
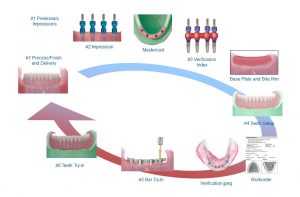
If master cast accuracy is verified and the laboratory receives the proper information on the bite registration, they we are ready for a tooth try-in. The clinician will then check for proper occlusion, shade and esthetics. One approved, the hybrid bar is milled, the tooth set up is then transferred to the hybrid bar and tried in one more time to verify fit and bite. After approval, the case is then processed and finished and inserted.
It is extremely important that patients follow proper guidelines for hygiene. Regular check-ups are recommended every 6 or 12 months to avoid complications and to assess the status of the tissue around the implants and occlusion. The measurement of radiographic implant marginal bone loss during the follow-up period is also recommended. There are many other material choices for hybrid type restorations but proper cases planning and communication among all parties is a prescription for success.
About the Author:
Dennis Urban, CDT brings 40+ years of dental technology field experience including lab management, technical training, sales and marketing, product development, and quality assurance. In addition to being a seasoned dental lab manager, Dennis has been an eminent lecturer worldwide since 1985. His lectures and trainings span many areas of dental technology, to include: denture set-ups, digital technology, denture processing, lab management, implant overdentures and bar design protocol, all on 4 and 6 case planning, chairside conversions, shade communication, occlusion and soft liners. His technical articles have been published in publications across the US, Canada and Europe. Dennis Urban is the current Chair of The National Board of Certification In Dental Technology, and is Technical Advisor and General Manager for Dental Services Group (DSG).







If you are looking for reliable dental treatment in the US I would recommend the services offered by https://www.advanceddentalgermantown.com/dental-services
Hello Dennis, Great article! I should mention I am a patient and not in the dental field. I have a question and I hope you can give me some advice! Your reply would mean a great deal to me!
I am in the process of having dental work done. I wasn’t an edentulous patient, but before my treatment I had broken down teeth down to the root, so my vdoo was lost, and I think I had a class 2 or 3 malocclusion.
I am currently in a all on five bottom temp, and in a top denture temp with bone grafting in each socket. I am currently going for my wax try in’s for my top denture, and need to sign off on it before they start making my zirconia bridge. My question to you is, is it important to have both arches made at the same time when doing this procedure and before putting my in a top permanent piece? And if one was to be finished before the other, would it be the lower arch? I recently got a 2nd opinion from a lab in my area, evaluated my situation, and explained that there will not be a positive outcome if my dentist proceeds to finish my top denture before putting me in a second protocol on the bottom arch as it will have a less pleasing esthetic effect as well as not having corrected my vertical dimension of occlusion. Keep in mind I went for the second opinion because I felt in my gut something wasn’t right! I do not like the teeth they made up of me, and the bottom temp is so narrow, it is not filling out my jaw as well as giving me the “denture face” look! I am young and with all the research I have read since I have been saving for the years I have been saving for this procedure, taught me that proper pre-treatment planning and proper measurements is a must for a esthetically pleasing face/smile!
Thank you so much for your time! Your advice is soooo greatly appreciated!!
Ms. Collapsed bite.
Great information you have here. This is very helpful to those hesitant to undergo implants.
Great article and thank You for Providing Such a Unique and valuable information. also, you can visit
Crown Dental Care
The hybrid denture procedure is indeed complex. A detailed explanation like this is very useful for both students and practitioners. Very inspiring.