INTRODUCTION
Making the emergence profile around implants cleansable is a highly desirable characteristic for a successful implant restoration. With an increased demand for esthetic implant restorations, especially in the anterior, effective management of the soft tissue and the emergence profile is critical. In addition to being esthetic, proper contouring of the peri-implant soft tissue helps maintain adequate peri-implant health and provides better access for hygiene. These factors can significantly improve the long-term prognosis of the restoration. This emergence profile and contour of the soft tissues can be maintained after implant placement in post-extraction sockets via the fabrication of an immediate provisional restoration. The fabrication of an immediate provisional depends on many factors such as occlusion, patient compliance, and mechanical factors like primary stability.1,2,3 If the implant cannot be immediately provisionalized, a custom-made healing abutment can maintain the soft tissue architecture. In cases where the implant is left to heal with no prosthetic component connected to it, the clinician will work on the emergence profile of the restoration during the provisionalization phase.4
There are several methods to replicate and transfer the soft tissue contour to the working cast and eventually the final restoration, including either the direct or the indirect technique. The direct technique involves sculpting the patients’ gingiva intraorally via the utilization of a provisional restoration. The soft tissue is manipulated with the interim restorations, allowing it to mature, and a final impression is made with the sculpted soft tissue. This results in an increased chairside time and requires precision on the clinicians’ part. It may also require the use of anesthesia and a period of time for the gingiva healing. Once the desired soft tissue contour is achieved, this information is transferred to the laboratory for fabrication of a final restoration with the desired emergence profile.5,6
In the indirect technique, the gingival molding or sculpting is achieved on the soft tissue cast in the laboratory, and a custom-made healing abutment, provisional or final restoration is fabricated over the soft tissue cast.7 At the time of delivery of the provisional or final restoration intra-orally, transient blanching of the soft tissue may ensue. It is important that this pressure is not excessive to prevent adverse tissue effects.4 The pontic design or emergence profile of the restoration must then be modified to avoid excessive pressure on the soft tissue. Most often clinicians prefer a combination of the two techniques. The soft tissue is modified to the desired contour in the lab and then the gingiva is reshaped to match the provisional restoration.
Some other ways of achieving the desired soft tissue contour include using a customized healing abutment prior to making the final impression or making an intra-oral scan of the implant and the surrounding soft tissue and then fabricating a working soft tissue cast.8-10 Regardless of the technique used, restorations that support the underlying soft tissue will result in esthetically pleasing restorations.11 This is particularly important in patients with a high smile line who display the junction of the implant abutment interface.
A soft-tissue cast is therefore highly desirable for implant restorations. It allows the laboratory technician to remove the soft tissue and get direct access and visualization of the implant abutment connection. Additionally, it allows the prosthesis to be fabricated over the implants or abutments with ease and ensures an accurate fit at the connection without the interference of the gingiva. It also helps simulate the gingiva around the implant and allows the technician to fabricate the restoration without the stone around the implant fracturing. A soft tissue cast or gingival mask around implants allows the laboratory technician to manipulate it if needed to achieve the desired emergence profile for the restoration. A gingival mask must also have a good tear strength and be easy to trim. From a clinicians’ perspective, it reduces chairside time and provides an esthetically pleasing restoration with minimal adjustments to the contour of the restoration.
Advancements in digital technology have made it easy to scan casts, digitally design, and fabricate implant restorations. In these situations, a soft tissue cast is still desired. When the cast is scanned, the gingival mask is often removed to allow an accurate scan of the implant abutment connection to be made. A second scan with the gingival mask in place is made and the two are superimposed to achieve the desired contours to fabricate the restoration. Most of the commonly used soft tissue masks, however, do not scan adequately. They often require the use of a contrast spray such as titanium oxide to show up accurately on a scan, and even when used, do not always result in an accurate scan. The desired characteristics of a gingival mask are listed in Table 1.
To the knowledge of the author, there isn’t any article comparing the scannability of different silicones for soft tissue implant casts. In this study, the three most commonly used soft tissue materials were compared to the scan of a stone model which was used as the control. The purpose of this study is to evaluate the feasibility of scanning of three gingival masks and to compare the scan to that of the stone cast.
MATERIALS and METHODS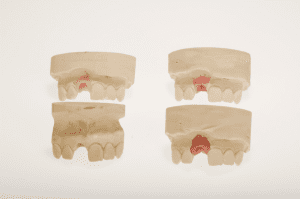
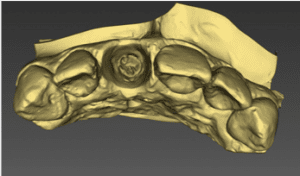
A single implant polyvinyl siloxane impression was used. An implant replica with a 3.5 mm platform diameter (Zimmer Tapered Screw Ventâ) was attached to the open tray impression and stone cast was poured in dental stone (Type IV). The solid stone cast served as the control. The stone cast was duplicated and the gingival emergence profile was replicated with each of the three soft tissue materials. Three types of addition silicones used specifically for replicating the gingival emergence profile were scanned using a desktop scanner, and the scans were compared. The materials used were GC (Gingifast CAD Elastic, Zhermack), GT (GingitechTM, Ivoclar Vivadent), and SM (Soft tissue moulage, Kerr) (Fig. 1). A scan was made of each cast using a desktop lab scanner (inEoX5, Dentsply Sirona). An anti-glare spray (Renfert Scanspray) was applied to the casts with GT and SM gingival masks and a second scan was obtained of these two materials (Figs. 2-5). All scans were visually analyzed.
Figure 2 a,b,c:

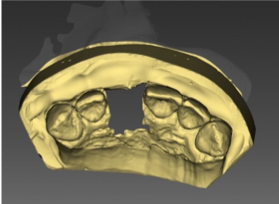
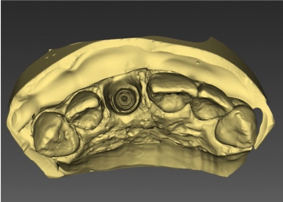
Figure 3 a,b,c:

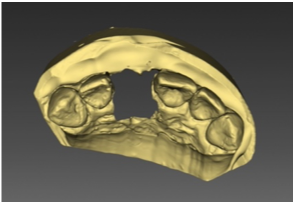
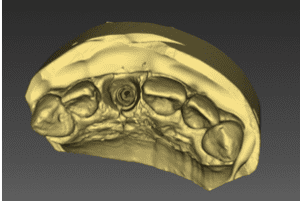
Figure 4 a,b:

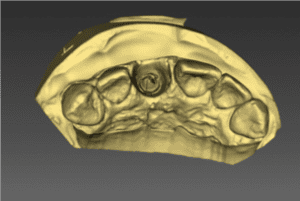
Figure 5 a,b:

RESULTS
The GT and SM soft tissue materials did not show on the scan without the contrast spray. The Gingifast CAD Elastic cast resulted in a scan that was visually similar to the control. It did not require the contrast spray.
DISCUSSION
The replication of the emergence profile is important for the fabrication of ideal restorations. If this is accomplished, the restorations made will deliver the outcomes that will satisfy both the soft tissue and tooth esthetics of implant supported restorations.12-14 For this to happen, the communication between the laboratory and the clinician must be efficient.15 It has been described in the literature that scanned dental casts are accurate and that the use of antiglare spray may help the scan become even more accurate.16 Nevertheless, the antiglare spray is not used in all the cases. Laboratory technicians on many occasions don’t use it as the scanners will capture the image of the gingival mask material without the need of spray. In this study, however, the GT and SM gingival masks did not show on the scan at all without the contrast spray. This means that these materials cannot be used without the antiglare spray. It is therefore important to know the properties of the material used to fabricate a soft tissue cast. The use of an antiglare spray is an additional step that results in increased laboratory time. The amount of spray applied to the soft tissue cast is critical. If too much spray is applied, it can incorporate inaccuracies in the scan. This is especially important for full arch implant soft tissue casts. Precise scanning techniques must performed to duplicate the emergence profile captured in the impression.17
CONCLUSION
The laboratory technician and clinician must understand the type of gingival mask being used, especially if the soft-tissue cast is going to be scanned to digitally fabricate an implant restoration. A gingival mask that does not require the use of a contrast spray is easier to scan and may result in a more accurate scan. This is particularly important in full arch implant restorations. It can also save valuable laboratory time.
About the Authors:
Dr. Faye Mascarenhas, David Tran, MCDT and Dr. Jonathan Esquivel are Assistant Professors, Dept. of Prosthodontics at Louisiana State University, School of Dentistry, New Orleans, LA
Edwin Kee, MCDT is an Associate Professor, Dept. of Prosthodontics, Louisiana State University, School of Dentistry, New Orleans, LA
Dr. Alika Yu is a Clinical Associate Professor, Dept of Prosthodontics, Louisiana State University, School of Dentistry, New Orleans, LA
References
1 Kan JYK, Rungcharassaeng K, Deflorian M, Weinstein T, Wang HL, Testori T.
Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000 2018;77:197-212.
2 Ottoni JMP, Oliveira ZFL, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants 2005;20:769-776.
3 Douglas de Oliveira DW, Lages FS, Lanza LA, Gomes AM, Queiroz TP, Costa Fde O. Dental Implants With Immediate Loading Using Insertion Torque of 30 Ncm: A Systematic Review. Implant Dent 2016;25(5):675-83.
4 Wittneben JG, Buser D, Belser UC, Brägger U. Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: the dynamic compression technique. Int J Periodontics Restorative Dent 2013;33:447-55.
5 Hinds KF. Custom impression coping for an exact registration of the healed tissue in the esthetic implant restoration. Int J Periodontics Restorative Dent 1997;17:584-91.
6 Vasconcellos F, Proussaefs P. A Technique for Duplicating the Contours of an Interim Implant Supported Crown to Fabricate a Custom Impression Coping and the Definitive Prosthesis. Implant Dent 2016;25:861-5.
7 Conejo J, Atria PJ, Hirata R, Blatz MB. Copy milling to duplicate the emergence profile for implant-supported restorations. J Prosthet Dent 2019 Sep 30. pii: S0022-3913(19)30414-7. doi: 10.1016/j.prosdent.2019.05.035. [Epub ahead of print]
8 Ruales-Carrera E, Pauletto P, Apaza-Bedoya K, Volpato CAM, Özcan M, Benfatti CAM. Peri-implant tissue management after immediate implant placement using a customized healing abutment. J Esthet Restor Dent. 2019 Jul 3. doi: 10.1111/jerd.12512. [Epub ahead of print]
9 Akin R. A new concept in maintaining the emergence profile in immediate posterior implant placement: the anatomic harmony abutment. J Oral Maxillofac Surg. 2016;74:2385-92.
10 Stumpel LJ, Wadhwani C. A customized healing abutment for immediate and delayed implant cases. Compend Contin Educ Dent 2017;38:672-78.
11 Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin. Oral Impl Res 2005;16: 639–44.
12 Hof M, Umar N, Budas N, Seemann R, Pommer B, Zechner W.Evaluation of implant esthetics using eight objective indices-Comparative analysis of reliability and validity.Clin Oral Implants Res. 2018 Jul;29(7):697-706. doi: 10.1111/clr.13261. Epub 2018 May 27.
13 Pollini A, Morton D, Arunyanak SP, Harris BT, Lin WS. Evaluation of esthetic parameters related to a single implant restoration by laypeople and dentists. J Prosthet Dent. 2019 Nov 18. pii: S0022-3913(19)30547-5. doi: 10.1016/j.prosdent.2019.08.017. [Epub ahead of print]\
14 Boon L, De Mars G, Favril C, Duyck J, Quirynen M, Vandamme K.Esthetic evaluation of single implant restorations, adjacent single implant restorations, and implant-supported fixed partial dentures: A 1-year prospective study. Clin Implant Dent Relat Res. 2020 Jan 7. doi: 10.1111/cid.12882. [Epub ahead of print]
15 Esquivel J, Tran David, Kee E, Mascarenhas F. The role of effective treatment planning and execution of anterior implant restorations: A restorative team approach. J Dent Technol 2019;36(9):26-32.
16 Peng L, Chen L, Harris BT, Bhandari B, Morton D, Lin WS. Accuracy and reproducibility of virtual edentulous casts created by laboratory impression scan protocols. J Prosthet Dent. 2018 Sep;120(3):389-395. doi:10.1016/j.prosdent.2017.11.024. Epub 2018 Apr 25.
17 Matta RE, Adler W, Wichmann M, Heckmann SM. Accuracy of impression scanning compared with stone casts of implant impressions. J Prosthet Dent 2017;117:507-12.







Thank you for sharing this post. For more information, visit our website https://www.verobeachartofdentistry.com/
Great read. Cast scans are an important part of diagnosing broken bones. However, casts made of soft tissue can be difficult to scan and read accurately. In a study, researchers attempted to determine the scannability of different types of soft tissue casts. They found that while plaster casts were easy to scan and interpret, silicone and rubber casts were not. The results of this study could help improve the accuracy of cast diagnoses.
Very informative post. Cast scanning is a common tool used in orthopedics to diagnose and track the progress of musculoskeletal injuries. While casts are often thought of as being made of hard materials, such as plaster or fiberglass, they can also be made from soft materials, such as cotton or neoprene. Soft tissue casts have several advantages over traditional hard casts, including increased comfort and scannability. This is important for diagnosing and tracking injuries. Does it allow physicians to see how the injury is healing over time?
Great Blog post. Thanks for sharing, you can also visit Crown Dental Care